Shocking Truth About Fibromyalgia: 17 Must-Know Facts for 2025
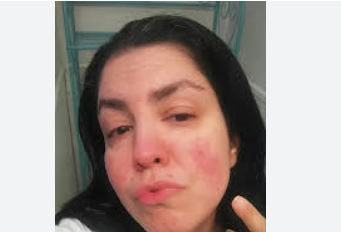
What is Fibromyalgia?
Fibromyalgia
is a long-term, chronic condition that causes
widespread pain throughout the body, accompanied by fatigue, sleep
disturbances, and cognitive issues. Often misunderstood or misdiagnosed, this
disorder affects millions globally, yet its precise cause remains elusive.
Despite not being visibly detectable through traditional medical tests, fibromyalgia is a very real and serious medical issue that can deeply
affect the quality of life.
The term itself combines two Latin
and Greek roots: "fibro" for fibrous tissues, "myo" for
muscles, and "algia" for pain. Together, they define the essence of
the disorder — persistent pain in muscles and soft tissues.
Understanding the Core Symptoms
One of the hallmarks of fibromyalgia is the widespread, persistent musculoskeletal pain that
doesn't seem to go away. However, this condition is about much more than just
discomfort. Patients often report a host of associated symptoms, including:
- Chronic fatigue, regardless of sleep duration
- Cognitive dysfunction or "fibro fog"
- Sleep disturbances, such as insomnia or non-restorative
sleep
- Sensitivity to noise, temperature, lights, or touch
- Headaches and migraines
- Irritable bowel syndrome (IBS)
- Depression and anxiety
- Numbness or tingling in the extremities
Who Is Most at Risk?
Fibromyalgia
can affect anyone, but it tends to be more common in women, particularly those
aged between 30 and 60. Genetics may play a role, especially when there's a
family history of the condition. Those with autoimmune diseases such as lupus
or rheumatoid arthritis are also at higher risk. Emotional trauma, severe
stress, or physical injuries may act as triggers in predisposed individuals.
Unraveling the Causes
While the precise cause of fibromyalgia remains unknown, researchers believe it's the result of
abnormal sensory processing in the central nervous system. Essentially, the
brain and spinal cord in people with fibromyalgia
may amplify pain signals or misinterpret non-painful stimuli as painful.
Other possible contributing factors
include:
- Genetic mutations or hereditary factors
- Imbalances in neurotransmitters such as serotonin and
dopamine
- Altered sleep cycles
- Past physical or emotional trauma
- Chronic stress or infections
Diagnosing Fibromyalgia Today
There is no definitive lab test for fibromyalgia, which makes diagnosis a challenging process. Doctors rely
heavily on patient-reported symptoms, medical
history, and physical exams. The most common diagnostic criteria include
experiencing widespread pain for more than three months and ruling out other
health conditions that could explain the symptoms.
In the past, doctors used a tender
point test, examining 18 specific spots on the body for pain response. However,
modern criteria have evolved to include broader symptom analysis and the use of
tools like the Widespread Pain Index (WPI) and Symptom Severity Scale (SSS).
Fibromyalgia
vs. Other Conditions
It’s important to distinguish fibromyalgia from other chronic illnesses with overlapping symptoms. Conditions like rheumatoid arthritis, lupus, chronic
fatigue syndrome, and multiple sclerosis often share similar signs but have
different underlying causes and treatments.
Unlike autoimmune diseases, fibromyalgia does not cause inflammation or joint damage. Yet, the symptoms can be just as debilitating, which is why it's often grouped
under central sensitivity syndromes.
Modern Treatment Options
Though there is no cure for fibromyalgia, various treatments
can help manage symptoms and improve
quality of life. A combination of medication, lifestyle changes, and therapy
typically forms the foundation of treatment.
Medications Include:
- Antidepressants like amitriptyline and duloxetine
- Anti-seizure drugs like pregabalin and gabapentin
- Pain relievers (non-opioid preferred)
- Sleep aids and muscle relaxants
Therapies May Involve:
- Cognitive Behavioral Therapy (CBT)
- Physical therapy and occupational therapy
- Counseling and mental health support
- Biofeedback and mindfulness-based therapies
Diet and Lifestyle Adjustments
Many patients report symptom relief
through proper diet and regular physical activity. While there's no single “fibromyalgia diet,” common recommendations include:
- Anti-inflammatory foods (like leafy greens, berries,
and omega-3 rich fish)
- Avoiding processed sugars and refined carbs
- Staying hydrated
- Limiting caffeine and alcohol
Low-impact exercise such as walking,
swimming, and yoga is often beneficial. Consistency is key, even when fatigue
is high.
The Role of Stress Management
Stress plays a major role in
triggering and worsening fibromyalgia
symptoms. Learning to manage stress through techniques like deep
breathing, guided imagery, meditation, and progressive muscle relaxation can
significantly reduce flares.
Creating a daily routine that
includes downtime, setting limits, and practicing mindfulness are essential
strategies in long-term management.
Sleep Strategies That Work
Sleep disturbances are one of the
most frustrating aspects of fibromyalgia.
Even after a full night's rest, many patients wake up feeling exhausted. Here
are some ways to improve sleep:
- Stick to a consistent bedtime
- Limit screen time before bed
- Use calming rituals like warm baths or soothing music
- Avoid large meals or stimulants in the evening
- Create a comfortable sleep environment with minimal
noise and light
Living With Fibromyalgia
Living with fibromyalgia means making adjustments, but it doesn’t mean giving up.
Many people with this condition lead full, satisfying lives. It’s about finding
what works for you, whether that’s a specific treatment, support system, or new
daily routine.
Support groups, whether online or
in-person, offer encouragement and advice from those who truly understand the
journey.
FAQs About Fibromyalgia
1. Is fibromyalgia a real disease or just in the mind?
Fibromyalgia is very real. It's recognized by major medical
organizations worldwide. While it involves the nervous system, it is not a
psychological disorder.
2. Can fibromyalgia be cured?
There is no known cure yet, but symptoms can be
effectively managed through lifestyle changes and medical treatment.
3. Is fibromyalgia considered a disability?
In many cases, yes. If it significantly limits your ability to work or perform
daily tasks, it may qualify as a disability under certain guidelines.
4. How is fibromyalgia different from arthritis?
Unlike arthritis, fibromyalgia
does not cause joint inflammation or damage. The pain is in muscles and soft
tissues rather than bones and joints.
5. Can children or teenagers get fibromyalgia?
Yes, although rare, fibromyalgia
can develop in adolescents and is known as juvenile primary fibromyalgia syndrome.
6. Is exercise safe for fibromyalgia sufferers?
Yes, gentle and consistent exercise often helps reduce symptoms, improve sleep, and boost mood.
Conclusion
Understanding what is fibromyalgia is the first step toward taking back control. Though
challenging, this condition doesn’t have to define your life. Through a
combination of medical treatment, lifestyle changes, and emotional support,
it’s possible to live well with fibromyalgia
in 2025 and beyond. As research progresses and awareness grows, so too will the
hope and resources available to those affected.
Click here to buy this or visit fibromyalgia store
For More Information Related to Fibromyalgia Visit below sites:
References:
Join Our Whatsapp Fibromyalgia Community
Click here to Join Our Whatsapp Community
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores










Comments
Post a Comment